Peripheral Artery Disease
Under Construction
Peripheral Artery Disease
Percutaneous Coronary Intervention
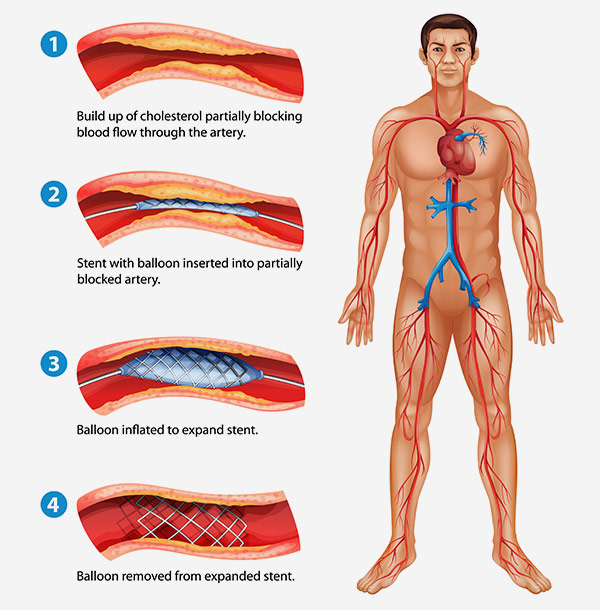
Percutaneous coronary intervention (PCI), also known as Cardiac Catheterization, is a procedure to open blocked coronary arteries and restore blood flow to the heart muscles. PCI is one of many treatment options available to you and your physician. Other treatments include lifestyle changes, medication, and surgery.
PCI is a minimally invasive surgical option. The procedure is performed in a cardiac catheterization laboratory (cath lab) by a cardiologist with specialized interventional training. The cath lab contains x-ray equipment which allows the interventional cardiologist to diagnose and treat coronary artery disease with only a small incision in the patient’s wrist or groin.
During the procedure, the patient is treated with medications that offer sedation and pain management but do not put the patient to sleep. Once the patient is comfortable, the physician makes a small incision in the groin or wrist to gain access to the patient’s arterial system. From that incision point, the physician delivers specialized instruments to the coronary artery designed to open the blockage and restore blood flow. In many cases, the physician will also place a stent at the site of the blockage. This stent is designed to keep the artery open while it heals from the procedure.
Stents are small, mesh tubes that are placed in the artery during a PCI procedure to prop it open during healing and recovery. Most patients are treated with metallic, drug-eluting stents. These stents are made from a metal alloy and coated with a drug. After the stent is placed in the artery, the drug elutes into the vessel wall to reduce vessel narrowing during healing. Over time, the stent heals into the artery wall where it remains as a permanent implant for life.
Bioresorbable Scaffolds
Bioresorbable scaffolds (BRS) are designed as an alternative to metallic stents to prop open the artery after PCI. Bioresorbable scaffolds are made from a biodegradable material and coated with a drug. After a scaffold is placed in the artery, drug elutes into the vessel wall to reduce vessel narrowing during healing. Over time, the bioresorbable scaffold heals into the artery wall and then degrades and resorbs from the body, without leaving a permanent implant behind.
While patients often feel relief from symptoms immediately following PCI, the treated artery takes three to six months to heal. Once the artery is healed, it no longer requires the support of the stent or scaffold. Bioresorbable scaffolds are designed to disappear (or “resorb”) from the body over time. This resorption is intended to allow the return of natural movement and function to the artery.
Recovery
Most patients feel relief from symptoms immediately following PCI. This is great because it’s time to start recovery. Many hospitals and health care systems offer programs to improve your heart health. Talk to your health care provider about options that are available to you.
Medication
Your doctor will prescribe blood thinning medications for you to take following your procedure. These medications are designed to reduce the risk of blood clots forming on your new stent or scaffold. It is important to comply with your doctor’s instructions with these medications.
Additionally, your doctor may prescribe medications designed to improve your heart health. These include medications to control blood pressure, blood sugar, and blood cholesterol levels. Taking these medications, along with lifestyle changes, can slow the progression of cardiovascular disease and reduce the likelihood of PCI in the future.
Lifestyle Changes
Regular exercise and a heart-healthy diet can improve heart health. The American Heart Association (AHA) recommends 40 minutes of aerobic exercise three to four times a week1. Walking is a great form of cardiovascular exercise!
An AHA, heart-healthy diet includes whole foods such as fruits and vegetables, lean meats, and whole grains. Avoid foods that are high in sugar and saturated fats2. There are a lot of resources to learn about healthy eating.
Remembering to take medication and making lifestyle changes can be challenging. The rewards can be immense: more time and energy to spend with loved ones, engage in work or hobbies, and enjoy life.
Talk to your doctor before embarking on exercise programs, diets, or other lifestyle changes.
Check-ups
Regular check ups with your doctor are a great time to track your progress and discuss any successes and challenges you face during recovery. Your doctor will want to hear about any changes in symptoms and how you are responding to medication and lifestyle changes. Your doctor may be able to help by adjusting medications or recommending programs to help you achieve your goals.
Is a Bioresorbable Scaffold Right for You?
Fantom and Fantom Encore have CE Mark only. Fantom and Fantom Encore are available in select countries that accept CE Mark. Fantom and Fantom Encore are not available in the U.S. or countries that do not accept CE Mark.
Bioresorbable scaffolds are a newer treatment option compared to metallic stents. Unlike metallic stents, which are a permanent implant, bioresorbable scaffolds are designed to disappear (or “resorb”) from the body over time. This resorption is intended to allow the return of natural movement and function to the artery. Bioresorbable scaffolds have not been studied as extensively as metallic stents and are not appropriate for all patients. Talk to your doctor about whether a bioresorbable scaffold is right for you.
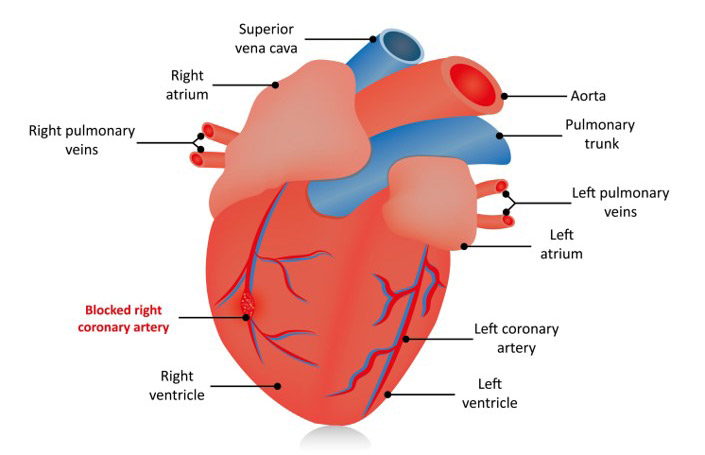
Your doctor will consider multiple factors when recommending a treatment plan and the use of a bioresorbable scaffold. These factors include availability of clinical trial data, location and severity of blockage in the coronary artery, and your total health condition.
Consideration for Appropriateness of BRS
- Age
- Presence of other health conditions such as kidney disease
- Ability to tolerate blood thinning medication
- Location and severity of blockage in the coronary artery
All procedures come with risks. It is important that you discuss potential risks and complications with your physician.
Learning about coronary artery disease is the first step in improving your heart health. We wish you all the best in your journey.
References:
- American Heart Association: http://www.heart.org/
- American Heart Association: https://healthyforgood.heart.org/eat-smart/articles/how-to-eat-healthy-without-dieting